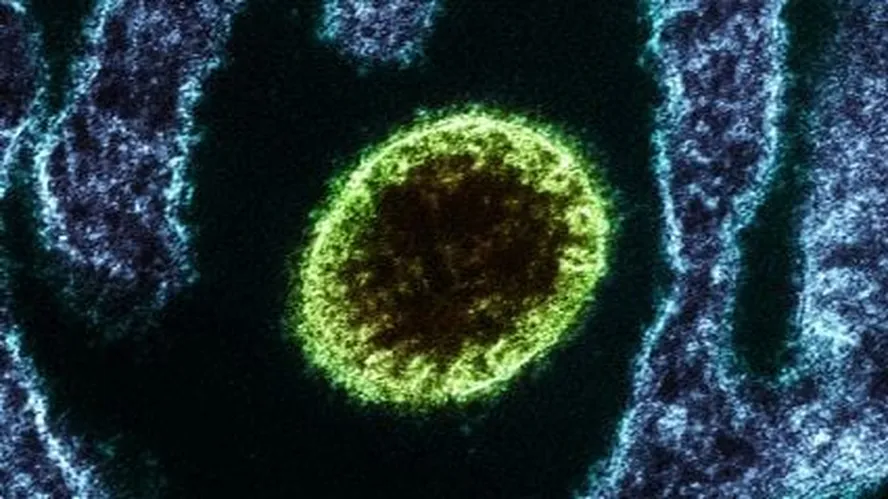
The recent detection of Nipah virus infections in eastern India has renewed international concern about this little-known but highly lethal zoonotic pathogen. Although the number of confirmed cases remains limited, health authorities and infectious disease specialists are focusing on the biological behaviour of the virus, its modes of transmission and the broader implications for global public health.
Several of the newly identified infections occurred among healthcare workers at a hospital near Kolkata, highlighting the virus’s ability to spread within medical settings. Similar patterns have been observed during previous outbreaks in South Asia, reinforcing the need for heightened epidemiological surveillance and a deeper understanding of a pathogen classified by experts as a serious global threat.
A virus that primarily affects the central nervous system
According to specialists in infectious diseases in Spain, Nipah virus infection most commonly leads to encephalitis, a severe inflammation of the brain. The illness often begins with non-specific symptoms, such as fever or mild respiratory complaints, before rapidly progressing to neurological involvement with a high risk of death.
The virus was first identified in Malaysia in 1998, during an outbreak linked to pig farming. Since then, recurrent outbreaks have been reported mainly in India and Bangladesh, where the virus continues to circulate intermittently.
Nipah is a zoonotic virus, with fruit bats of the Pteropus genus serving as its natural reservoir. Transmission to humans can occur through direct contact with infected animals, via intermediate hosts such as pigs or horses, or through the consumption of food contaminated by bat secretions, including raw palm sap.
Human-to-human transmission and hospital exposure
Beyond animal-to-human transmission, Nipah virus has demonstrated the capacity for person-to-person spread, particularly in healthcare environments. Hospital-based transmission has been documented in several outbreaks, explaining why medical staff have been disproportionately affected in some instances.
The World Health Organization (WHO) reports that, during previous outbreaks in India and Bangladesh, a significant number of infections occurred among healthcare professionals and family members caring for infected patients. This characteristic raises concerns about containment, especially in settings where early diagnosis may be challenging.
High fatality rate and limited medical options
One of the most alarming aspects of the Nipah virus is its exceptionally high mortality rate, which ranges from 40% to 75%, depending on the outbreak and the healthcare resources available. Currently, there is no specific antiviral treatment or licensed vaccine for the disease.
Clinical management relies primarily on supportive care, including intensive treatment for neurological and respiratory complications. Experimental therapies, such as immunotherapies and antiviral agents originally developed for other viral infections — including remdesivir and ribavirin — have been explored, but evidence of their effectiveness remains limited.
Due to these constraints, the WHO has included Nipah virus on its list of priority pathogens requiring urgent research and development of medical countermeasures.
Incubation period and pandemic risk
The typical incubation period for Nipah virus infection is estimated to range from four to 14 days. However, specialists caution that if future evidence confirms longer incubation periods or transmission during asymptomatic phases, the virus’s potential for widespread international spread would increase substantially.
Such characteristics would complicate outbreak detection and control, particularly in a context of extensive global travel.
Assessing the risk beyond South Asia
Despite the current outbreak in India, experts indicate that the immediate risk to Spain remains low. Nevertheless, they acknowledge that international mobility makes the importation of rare infectious diseases theoretically possible.
Spain maintains specialised high-level isolation units designed to manage severe and highly infectious diseases, should a case be detected. Preventive strategies continue to focus on traveller awareness, hygiene measures and strict adherence to international health regulations.
Prevention and the One Health perspective
Public health authorities stress that prevention remains the most effective tool against Nipah virus infection. Recommendations include avoiding contact with potentially infected animals, consuming well-cooked food, and following official travel health advice when visiting regions with active outbreaks.
Experts also emphasise the growing relevance of the One Health approach, which recognises the interconnectedness of human, animal and environmental health. Increased human encroachment into wildlife habitats has been linked to the emergence of zoonotic diseases worldwide, underscoring the need for sustainable interaction with natural ecosystems.
As global attention returns to the Nipah virus, specialists agree that continued surveillance, international cooperation and investment in research are essential to reducing the risk posed by one of the world’s most dangerous emerging pathogens.