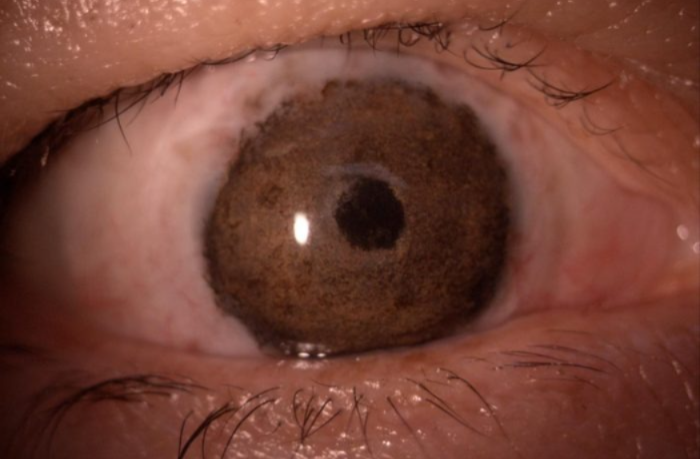
In Chile, an ophthalmic procedure known as corneal pigmentation, or keratopigmentation, is gaining attention as a therapeutic option for patients affected by severe corneal opacity. Although still relatively unfamiliar to the broader public, the technique has demonstrated significant potential in restoring the natural appearance of the eye and improving patients’ psychological and social wellbeing.
According to clinical observations reported by specialists in Chile, keratopigmentation involves the insertion of specially designed pigments into the corneal tissue to replicate the natural colour of a healthy eye. The method is primarily recommended for individuals with corneal scarring or opacity, conditions that can result from surgical complications, trauma, viral infections such as herpes simplex keratitis, or congenital disorders. In many cases, these patients have already lost visual function in the affected eye, but the visible alteration in eye appearance can lead to considerable emotional distress and social withdrawal.
Clinical Approach and Surgical Method
Ophthalmologists in Chile describe keratopigmentation as a minimally invasive intervention performed using specialised micro-needle instruments and biocompatible pigments developed specifically for ocular application. The process is typically guided by matching the pigmentation to the patient’s unaffected eye, aiming to achieve a symmetrical and natural visual outcome.
The procedure usually lasts between 30 and 40 minutes and is carried out under local anaesthesia, often accompanied by mild sedation supervised by an anaesthesiology professional. Clinical reports suggest that patients generally tolerate the intervention well, with limited discomfort during and after the surgery. Continuous comparison with the unaffected eye during the procedure is considered essential to optimise cosmetic results.
Therapeutic and Functional Applications
Medical specialists in Chile identify three principal clinical uses for keratopigmentation. The first involves cosmetic modification in otherwise healthy eyes, a practice that remains controversial and is not formally regulated in Chile. Some countries, including Brazil, have imposed restrictions on purely aesthetic ocular pigmentation procedures due to safety concerns.
The second clinical application addresses structural defects of the iris that may cause excessive light sensitivity, glare, and visual distortion. In these cases, pigmentation acts as a protective barrier, regulating the amount of light entering the eye and improving visual comfort.
The third and most widely accepted indication is therapeutic, focusing on patients with complete vision loss combined with corneal opacity. Here, the primary objective is to restore a more natural eye appearance, which can have a profound impact on psychological health and social reintegration.
Psychosocial Outcomes and Patient Wellbeing
Evidence emerging from clinical practice in Chile indicates that keratopigmentation may deliver benefits that extend beyond physical restoration. Patients undergoing the procedure frequently report improvements in self-esteem, social confidence, and overall quality of life. Ophthalmologists note that individuals who previously avoided public environments, employment opportunities, or social interactions due to visible ocular abnormalities often experience a significant return to daily activities following treatment.
Documented patient experiences highlight the psychological burden associated with ocular disfigurement, particularly in cases where previous interventions, including cosmetic contact lenses or multiple surgeries, have failed to achieve satisfactory results. The availability of keratopigmentation has provided an alternative solution for selected patients who previously had limited therapeutic options.
Recovery and Safety Considerations
Postoperative recovery following keratopigmentation in Chile is generally uncomplicated. Patients are usually discharged with a protective eye patch that is removed within 24 hours. Temporary sensitivity to light or mild irritation may occur during the initial recovery phase, and topical antibiotic and anti-inflammatory medications are routinely prescribed. Preventative antiviral therapy may also be recommended in certain clinical scenarios.
As with any surgical intervention, there are potential risks. Infection represents the primary complication, although reports suggest that severe adverse events remain uncommon due to the superficial nature of the procedure. In some instances, additional pigment adjustments may be required to refine colour matching after the initial healing period.
Specialist Training and Limited Availability
Despite its therapeutic promise, keratopigmentation remains a highly specialised procedure in Chile, performed by a limited number of ophthalmologists with advanced training in corneal diseases and ocular micropigmentation techniques. Medical professionals emphasise that the surgery should only be carried out in regulated clinical environments by qualified specialists, as unregulated procedures may expose patients to significant health risks.
Advancing Ophthalmic Rehabilitation
The growing adoption of keratopigmentation in Chile reflects broader advancements in ophthalmic rehabilitation, where the focus increasingly extends beyond visual restoration to encompass aesthetic and psychological outcomes. Scientific literature in corneal therapy continues to emphasise the importance of personalised treatment strategies for ocular surface disorders, supporting the integration of innovative techniques such as keratopigmentation into multidisciplinary patient care.
As awareness of the procedure expands, healthcare professionals in Chile continue to highlight the importance of clinical research, specialist training, and regulatory oversight to ensure patient safety and optimise therapeutic outcomes.